IT Band Syndrome Acupuncture San Diego: Why Standard Treatments Fail
In this blog post and video, I dive into the frustrating cycle of IT band syndrome, a common issue for runners that often stems from problems in the hip and pelvis rather than the knee itself. I explain how subtle imbalances in the pelvis can lead to a cascade of dysfunction, ultimately overloading the IT band. It's crucial to shift our focus from treating the symptom to addressing the root cause by restoring proper function to the hip stabilizers. I encourage you to assess your own running form and muscle activation, particularly in the glute medius, to identify any underlying issues. Remember, your IT band pain is a messenger, signaling that something else needs attention
⏱️ TIMESTAMPS:
0:00 - Understand IT Band Syndrome
0:25 - Identify Symptoms
0:39 - Avoid Common Mistakes
1:04 - Shift Your Mindset: IT Band as Victim
1:55 - Identify the Real Culprit: Hip & Pelvis
2:23 - Analyze Pelvic Imbalance
2:50 - Assess Hip Function
3:08 - Observe Running Form (Cross-Over Gait)
4:02 - Understand the Biomechanical Model & East-West Bridge
4:52 - Implement Solutions
5:19 - Conduct a Proper Assessment
5:58 - Seek Professional Help
The Mindset Shift: Your IT Band Is the Victim 1:04
For too long, we've blamed the IT band itself—attacking it with foam rollers, stretching it aggressively, treating it like the villain in your injury story. But what if it's not the problem at all? What if it's actually the victim?
The IT band is a thick fascial structure designed to handle tremendous tension—it's one of the strongest connective tissues in your body
When it becomes irritated or painful, that's not the IT band failing—it's being massively overloaded by dysfunction happening upstream
Think of it like a guy wire (stabilizing cable): when the structure it's supposed to stabilize is unstable, the cable pulls taut
Foam rolling is like mopping the floor while the sink overflows—temporary relief, but the water keeps coming
Stop punishing the messenger. Start finding the source.
The Real Culprit: Hip and Pelvis Dysfunction 1:55
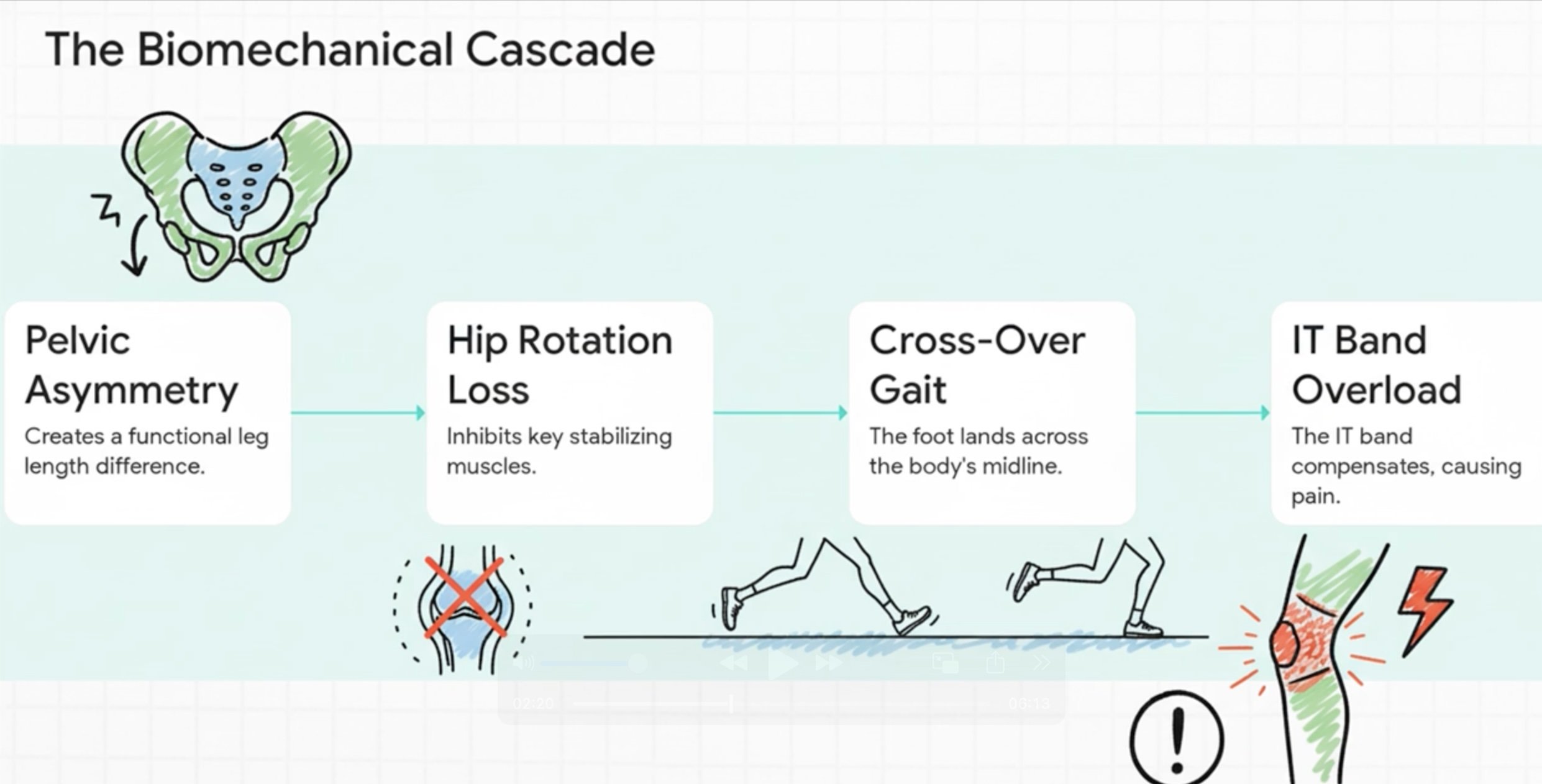
The evidence points upstream—to a cascade of dysfunction that starts at your hip and pelvis. This unfolds in a predictable four-step pattern that explains why your IT band pain keeps returning.
Pelvic asymmetry: Most runners develop a subtle twist or tilt in their pelvis from spending slightly more time on one leg during stance phase. This creates a "virtual long leg" on one side—not that the bone is longer, but your body has to act like it is with every step.
Hip rotation loss: To deal with that pelvic tilt, your body gives up internal rotation in the hip. Deep hip rotators (piriformis, obturators, gemelli) get tight and overactive. Worse, your key stabilizing muscles—glute medius and glute minimus—weaken or shut off completely.
Cross-over gait pattern: When those side hip stabilizers aren't doing their job, your pelvis drops every time you land on that leg. To prevent falling, your body compensates by making your foot land across the centerline of your body (cross-over gait). This creates abnormal torque and forces that your IT band has to resist with every stride.
Ground reaction force amplification: With cross-over gait, forces from the ground don't travel cleanly through your joint centers. Your IT band gets pulled taut trying to stabilize the mismatch. Multiply that stress by thousands of steps per run—that's your IT band pain.
This is why foam rolling alone never works. You're treating step 4 while steps 1-3 keep regenerating the problem.
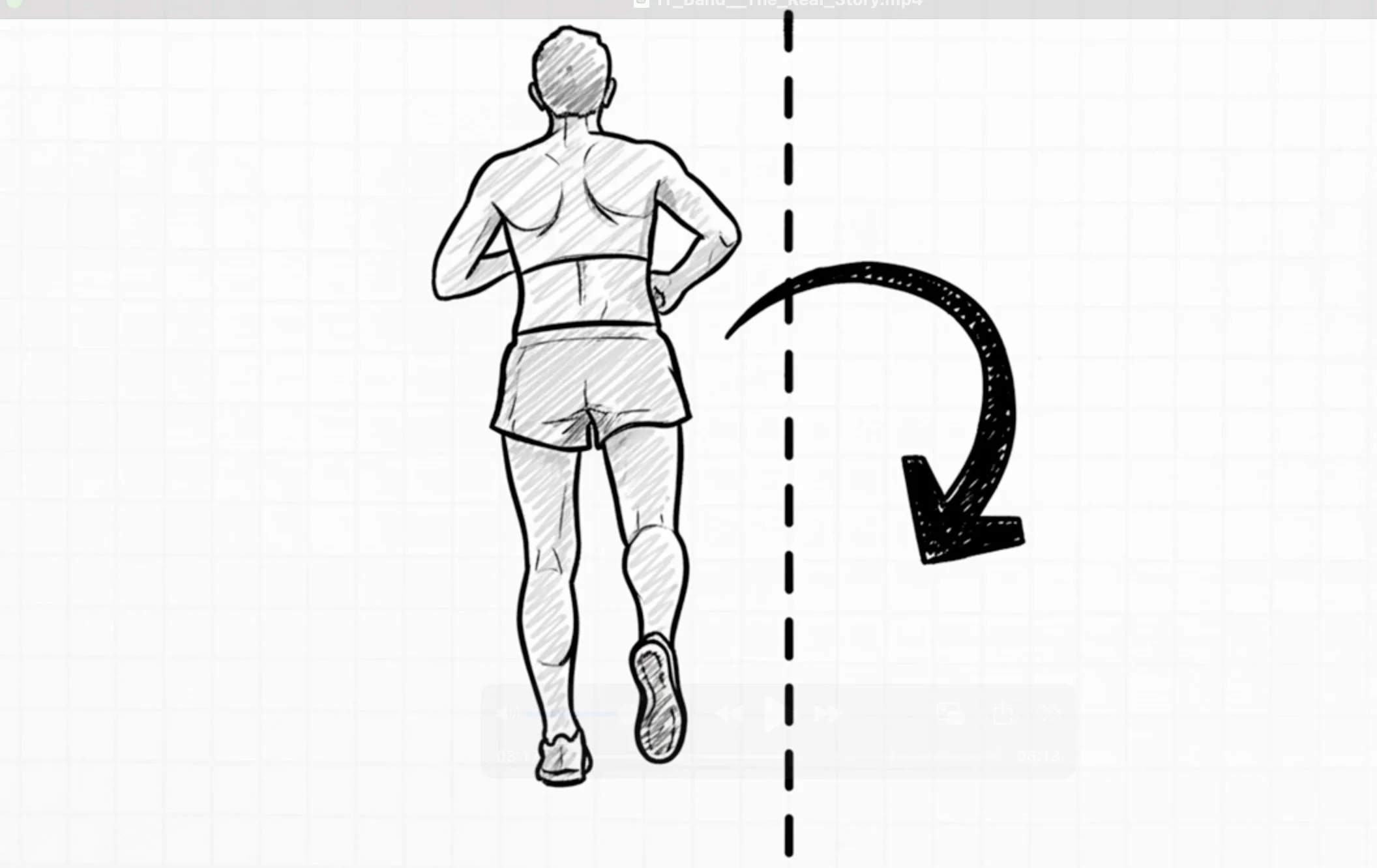
How It Shows in Your Running: The East-West Connection 3:08
When you understand both Western biomechanics and Eastern medicine, you see they're describing the exact same dysfunction from different perspectives.
Western view: Weak hip abductors (glute med, glute min) causing TFL and IT band overload. Your lateral chain (outside of leg) works overtime because your medial stabilizers (inside of leg) are weak.
Eastern view: Gallbladder channel excess (rigid, tight, overworked lateral line) compensating for Spleen channel deficiency (weak medial support, poor tissue integrity).
The bridge: Both describe a weak inside creating an overworked outside. Same imbalance, two complementary maps. Western explains the mechanical cascade. Eastern explains the energetic/functional pattern.
In your running, this shows up as: Cross-over gait where your foot lands medially across your midline, lateral hip tension that builds during runs, the feeling like you constantly want to stretch your IT band (because it's being pulled taut), and eventual sharp lateral knee pain that stops you in your tracks.
Ready to experience your first session? I offer complimentary 15-minute assessments where we can discuss your specific situation, answer your questions, and see if this approach makes sense for your training and recovery goals.
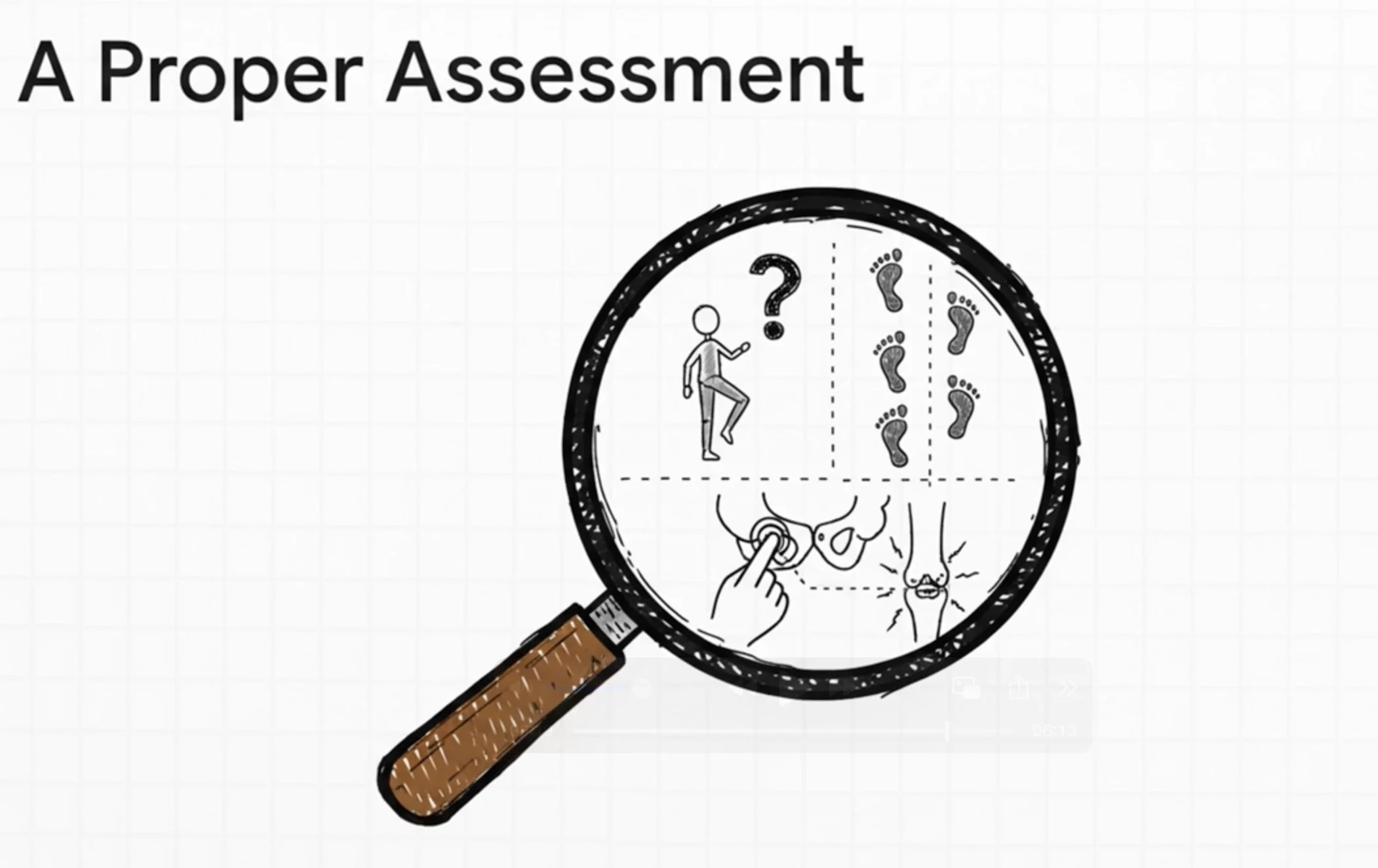
The Solution & What Assessment Reveals 4:52
If the problem starts at the hip and pelvis, the solution has to start there too. This is about restoring proper motor control to the muscles that should be stabilizing your pelvis so the IT band doesn't have to.
Assessment as detective work: Can you fire your glute medius in single-leg stance? Is cross-over gait visible when you run? Can we reproduce your exact knee pain by pressing a trigger point in your lateral hip? These clues reveal the specific pattern driving YOUR IT band pain.
Treatment integration: Motor point acupuncture with e-stim retrains the glute medius and glute minimus that have shut off (neuromuscular re-education). Trigger point release in TFL addresses the fascial restrictions creating pain referral. Channel work balances Spleen/Gallbladder to address the systemic pattern.
Why individual assessment matters: IT band syndrome isn't one-size-fits-all. Some athletes have purely hip-driven dysfunction. Others have foot mechanics contributing bottom-up. Many have both. Your training history, biomechanics, past injuries, and body type all influence which combination of factors is creating your lateral knee pain.
If you're tired of managing symptoms and ready to address the cause, assessment reveals what's actually happening in your body—not just general IT band advice, but YOUR specific pattern.
IT Band Syndrome Acupuncture San Diego: Why Standard Treatments Fail
You know the pattern. You're a distance runner, and the pain starts like clockwork. Around mile 3 or 4, subtle tightness appears on the outside of your knee. You push through, but by mile 6 it's sharp. By mile 8, you're done.
You rest a few days. Pain subsides. You run again—mile 3, it's back.
Foam rolling, stretching, compression sleeves—you've tried it all. The pain keeps returning, derailing your training and turning runs into anxiety-filled ordeals.
Here's why this cycle is so frustrating: standard treatments don't address the root cause. Your IT band is the victim, not the villain. The pain you feel at your lateral knee is a signal—a loud one—that your IT band is being massively overloaded by dysfunction happening upstream at your hip and pelvis.
Treating the site of pain is like mopping the floor while the sink overflows. You can manage the symptom temporarily, but until you turn off the faucet, the problem never truly goes away.
This post explores the hip and pelvic dysfunction pathway I see constantly in my San Diego practice that creates this overload. We'll look at it through both Western biomechanics and Traditional Eastern Medicine to reveal the complete picture. While other causes of IT band pain certainly exist—poor foot mechanics, training errors, direct trauma—this upstream pattern is so prevalent that understanding it is key for many runners to finally break the cycle.
If you're looking for effective IT band syndrome treatment with acupuncture in San Diego, understanding this connection is the first step.
Understanding IT Band Syndrome: The Overloaded 'Guy Wire'
In my San Diego practice, I see this pattern emerge like clockwork—typically weeks 9-12 of marathon training when weekly mileage crosses 40 or long runs push past 13-14 miles. This timing isn't random. It's the point where your body's compensation strategies can no longer keep up with training load.
Here's the fundamental misunderstanding that fuels ineffective treatment: The IT band isn't a muscle that gets "tight" and needs stretching. It's an incredibly thick, strong band of fascia—connective tissue—running from your hip down the outside of your thigh to your knee. It's one of the strongest connective tissues in your body, designed to handle enormous tension.
Think of it as a "guy wire" on a telephone pole. It's built for tension and provides lateral stability to your leg.
This "victim, not villain" framework is critical. When something that strong is screaming in pain, the underlying problem must be massive. The pain signals that this stabilizing guy wire is being pulled taut with excessive force—thousands of times per run—due to instability elsewhere in the system.
When your hip and pelvic muscles fail to control your leg during running, the IT band is forced to compensate. This leads to irritation and inflammation where it crosses the bony prominence of your knee.
This is why foam rolling offers only fleeting relief. You're temporarily loosening the messenger without addressing the source of the overload.
To truly solve the problem, we need to investigate the biomechanical cascade that created it:
Pelvic asymmetry → hip rotation loss → cross-over gait → IT band overload
The Western Biomechanics View: A Four-Step Cascade of Dysfunction
This is the mechanical breakdown of your kinetic chain. It reveals precisely how a subtle problem in your pelvis can manifest as sharp pain on the outside of your knee. Each step builds on the last, creating a predictable compensation pattern.
Mechanism 1: Pelvic Asymmetry
Running is repetitive single-leg activity. Over thousands of miles, most runners develop a slight bias, spending more time on one leg than the other during stance phase.
This creates a "stuck" pelvic pattern—one side held in a slightly different position than the other. The result? A functional or "virtual" leg length difference.
With one leg behaving as if it's longer, your body makes constant compensations just to stay balanced and keep moving forward.
Mechanism 2: Hip Rotation Loss
Normal running gait requires at least 5 degrees of hip internal rotation for proper loading and shock absorption. But in this dysfunctional pattern, the deep hip external rotators (like piriformis, obturators, gemelli) become tight and overactive.
In response, key stabilizers like gluteus medius and gluteus minimus—which help control hip internal rotation—become inhibited or effectively "shut off."
The femur can't rotate smoothly in the hip socket. Other structures are forced to compensate.
Mechanism 3: Cross-Over Gait Pattern
This is the visible running flaw you'd see on video. When your hip abductors (glute med, glute min) are weak or inhibited, they can't control your pelvis during single-leg stance.
Your pelvis drops on the swing leg side. To prevent falling, your nervous system compensates: it drives your stance leg medially, across your body's midline.
This "cross-over" gait puts immense, abnormal stress on all your lateral structures—especially the Tensor Fasciae Latae (TFL) and IT band.
Mechanism 4: Ground Reaction Force Amplification
With cross-over gait, forces from the ground no longer travel cleanly through the center of your joints. Instead, this inefficient pattern creates torques and lever arms at your ankle, knee, and hip.
To resist these abnormal forces and stabilize your leg, your IT band is pulled taut with every single stride.
Multiply that by thousands of steps per run. That cumulative overload is what leads to the friction, irritation, and inflammation at your lateral knee—the pain you experience as IT band syndrome.
The Eastern Medicine Perspective: Why Your Hip Dysfunction is a Channel Imbalance
While the biomechanical view is precise, it's not the only way to map this problem. Traditional Eastern Medicine offers a different but perfectly complementary perspective.
These channels aren't mystical concepts. They're anatomical, fascial pathways that describe functional relationships in your body.
The Gallbladder Channel (The Overworked Lateral Line)
The Gallbladder sinew channel is the fascial line Western anatomists call the "lateral line." It follows the exact pathway of the TFL and IT band, running from hip to lateral knee to fourth toe.
In runners with IT band syndrome, I observe this channel in a state of Excess. It feels tight, rigid, cord-like—almost like steel cable. This excess state shows up as inflammation and pain that worsens with activity.
Importantly, this excess is compensatory. The Gallbladder channel is working overtime because another system is failing to do its job.
The Spleen Channel (The Weak Medial Line)
The Spleen channel runs along the medial (inner) aspect of your leg—the "medial line." It starts at the big toe and anatomically tracks key medial stabilizers like vastus medialis oblique (VMO), adductors, and parts of gluteus medialis.
In IT band syndrome, this channel is typically in a state of Deficiency. It's weak, underactive, lacking the integrity to provide proper support.
Spleen channel deficiency manifests as poor stability, slow recovery from training, and a general tendency for tissues to break down.
The Connection
They aren't just similar—they're identical.
"Deficient Spleen channel" is the systemic pattern that results in inhibited medial stabilizers like glute medius. "Gallbladder channel in compensatory excess" is the palpable tension in an overworked TFL and IT band.
Two different languages describing the exact same dysfunctional relationship: medial weakness leading to lateral compensation.
The East-West Bridge: How Sports Medicine Acupuncture Sees the Complete Picture
By using both maps, we see the problem not just as a mechanical fault but as a systemic imbalance. The synergy between perspectives is where effective, lasting treatment comes from.
Here's how findings from each model map directly onto one another:
Western Finding: Gluteus medius inhibition → Eastern Map: Spleen channel supports deep hip stability
Western Finding: VMO weakness → Eastern Map: Spleen channel governs medial knee
Western Finding: TFL overactivity and IT band tension → Eastern Map: Gallbladder channel in compensatory excess
Using both maps is critical for complete diagnosis and effective treatment. Western mechanics tells us what is happening—which muscles are failing, how the kinetic chain is breaking down. Eastern medicine tells us why from a systemic view, explaining the underlying pattern of imbalance.
Revisiting the "Guy Wire" Analogy
The IT band is the guy wire. It's pulling taut because the structure it's meant to stabilize—your hip and pelvis—is unstable.
Foam rolling is like temporarily loosening that wire. It might feel better briefly, but as soon as you start running again, the underlying instability causes the wire to pull tight once more.
The only lasting solution? Fix the structural problem by restoring proper hip motor control and rebalancing the Spleen and Gallbladder channels.
My Treatment Approach for IT Band Syndrome in San Diego
Before any needles go in, I'm doing detective work. Successful treatment for IT band syndrome starts with precise assessment to confirm this hip-driven pattern is, in fact, the source of your pain.
Assessment: The Detective Work
Manual Muscle Testing: Can you fire your glute medius in single-leg stance? Most runners with IT band pain cannot. I check if key stabilizers like this and the VMO can activate and hold against pressure. For most runners with chronic IT band syndrome, these muscles have effectively "shut off."
Movement Assessment: I watch you move. Is cross-over gait visible? When you single-leg squat, does your knee collapse inward? These visible signs confirm the compensation pattern in action—often one you never realized you had.
Trigger Point Mapping: What surprises most athletes: when I press into their lateral hip around the greater trochanter, I can reproduce their exact lateral knee pain. This simple test is often the "aha" moment, demonstrating unequivocally that the problem originates in the hip. They thought the problem was in their knee—it's actually in their hip.
Channel Palpation: My hands can feel the difference between channels. I palpate the tight, cord-like "excess" quality of the Gallbladder channel along the IT band and the comparatively weak, empty "deficient" quality of the Spleen channel on your inner thigh.
Treatment: An Integrated Solution
Based on assessment findings, treatment addresses the dysfunction at every level: neurological, muscular, fascial, and systemic.
Motor Point Acupuncture: This is highly specific neuromuscular re-education. The goal is to ACTIVATE inhibited muscles (glute med, glute min) and CALM overworked ones (TFL).
I often use electrical stimulation (e-stim) on the needles in the glutes. The signal needs to be strong enough for your brain to remember "oh, this muscle exists and I can use it." We're not just needling a muscle—we're teaching your nervous system to fire it again.
Trigger Point Release: Using acupuncture needles, I release key trigger points in the TFL, glute med, and vastus lateralis that are referring pain directly to the lateral knee and locking the hip in a dysfunctional pattern.
Channel Balancing: I select specific acupuncture points to correct the systemic imbalance. This involves tonifying the Spleen channel to build medial support (using points like SP6, SP9, SP10) and sedating the Gallbladder channel to release lateral tension (using points like GB30, GB31, GB34).
Treatment Progression
Everyone's body is different, so there's no rigid timeline. However, care generally progresses through three stages:
Stage 1 (Relieve): Early in treatment, the focus is on reducing acute pain and inflammation at the lateral knee to get you comfortable. You'll notice the sharp lateral knee pain starting to ease, you can walk without limping, acute inflammation calms down.
Stage 2 (Restore): As treatment progresses over weeks, focus shifts to root cause work—retraining motor patterns, activating the glutes, rebalancing Spleen and Gallbladder channels. This is motor retraining, so your nervous system is learning new patterns. You'll notice you can single-leg squat without knee collapse, your gait feels more balanced, you can run without pain returning immediately.
Stage 3 (Elevate): Once function is restored, focus becomes maintenance and prevention, ensuring your body can handle heavy training loads without the old pattern recurring. Frequency is typically monthly or as-needed based on training load.
The timeline depends on: how long you've had the injury, your training load during treatment, compliance with corrective exercises, and your nervous system's adaptation speed. Some athletes progress quickly if they catch this early. Others need more time if the compensation pattern has been building for months or years.
In my practice, I can often feel Gallbladder channel congestion building 1-2 weeks before an athlete notices pain. That's the signal to address it before it becomes limiting.
Prevention and Training Integration: How Runners Can Address Hip Dysfunction
Armed with this understanding, you can take proactive steps to address the root cause.
The Prevention Window
As mentioned, IT band syndrome often appears predictably in marathon training cycles. The best time to intervene is when you notice early warning signs—"subtle tightness at mile 4" or a feeling that your pelvis is "off."
I use these concepts in my own marathon training. I know when my left glute med starts getting lazy because I can feel Gallbladder channel tension building in my lateral thigh before any knee pain shows up. That's my signal to address it before it becomes a problem.
Don't wait for sharp pain to sideline you.
Key Training Modifications and Exercises
Address Cross-Over Gait: Integrate single-leg balance work and glute activation drills into your routine. Exercises like clamshells, lateral band walks, and single-leg deadlifts are excellent for teaching your glute medius to fire and stabilize your pelvis.
Reduce Running on Cambered Roads: Constantly running on the sloped shoulder forces one side of your body into continuous lateral compensation, feeding the dysfunctional pattern.
Vary Your Surfaces: Too much time on hard, flat pavement creates repetitive stress patterns. Mixing in some trail running can help.
Modify, Don't Stop: During treatment, you often don't need to stop training completely. Cross-training activities like swimming or cycling maintain fitness without the repetitive impact that aggravates the injury.
Post-Long Run Treatments: Weekend appointments work perfectly for this. I can treat you post-long run when tissues are most reactive and compensation patterns are fully manifested. That's when I get the clearest picture of what's actually happening in your gait mechanics.
Conclusion: Your Path to Resolving IT Band Pain Starts at the Hip
To recap the core insight: for many distance runners, IT band syndrome isn't a knee problem. It's a kinetic chain problem that starts with pelvic and hip dysfunction, which creates a compensatory gait pattern that overloads the IT band.
Both Western biomechanics and Eastern channel theory point to the exact same pattern: medial weakness leading to lateral compensation.
While this hip and pelvic pathway is incredibly common, IT band syndrome isn't one-size-fits-all. Your specific pattern depends on unique biomechanics, training history, and other contributing factors from the foot and ankle up. Some athletes have purely hip-driven issues. Others have foot mechanics contributing. Many have a combination of both.
The only way to understand YOUR specific pattern is through proper assessment. If you've been stuck in the frustrating cycle of rest, foam rolling, and recurring pain, it's time to look at the source.
I offer complimentary 15-minute assessments at Funktion Acupuncture in San Diego where we can discuss your training, your symptoms, and your goals to determine if this integrated approach to IT band treatment San Diego is right for you.
This content was created with AI assistance (Claude AI & Google NotebookLM) and inspired by comprehensive patient experience documentation and clinical practice insights. All clinical perspectives and Eastern medicine explanations are from Michael Cohen, LAc, practicing sports medicine acupuncture in San Diego at Funktion Acupuncture.